Women who are diagnosed to have cancer recently-do they have options to preserve their fertility?
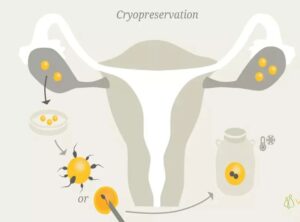
Ans: Yes, before treating the cancer, fertility experts can freeze.
1. Eggs,
2. Fertililised eggs called embryos or
3. The ovarian tissue by new technologies.
In this way women may produce babies once their treatment for cancer is completed. This process of freezing is called as cryopreservation.
Lymphomas, leukemias, breast cancer, thyroid cancers and gynecological cancers viz cervical cancer, uterine cancer or ovarian cancer are some of the most common cancers in girls and young women. They are treated with surgical approach or chemotherapy or by radiation or even by the combination treatment, as per the case may be. There are several factors that determine women’s fertility, after cancer treatment like age of women, location of radiation therapy, drugs used in chemotherapy. Cancer treatment can remarkably decrease women’s fertility by harming the quality or quantity of eggs.
Cryopreservation has proved to a boon for preserving fertility in such women.
Egg (oocyte) cryopreservation
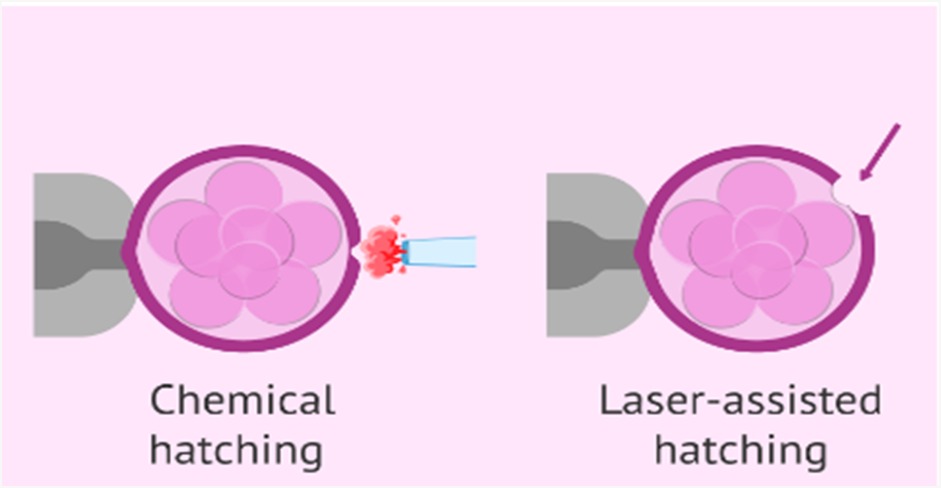
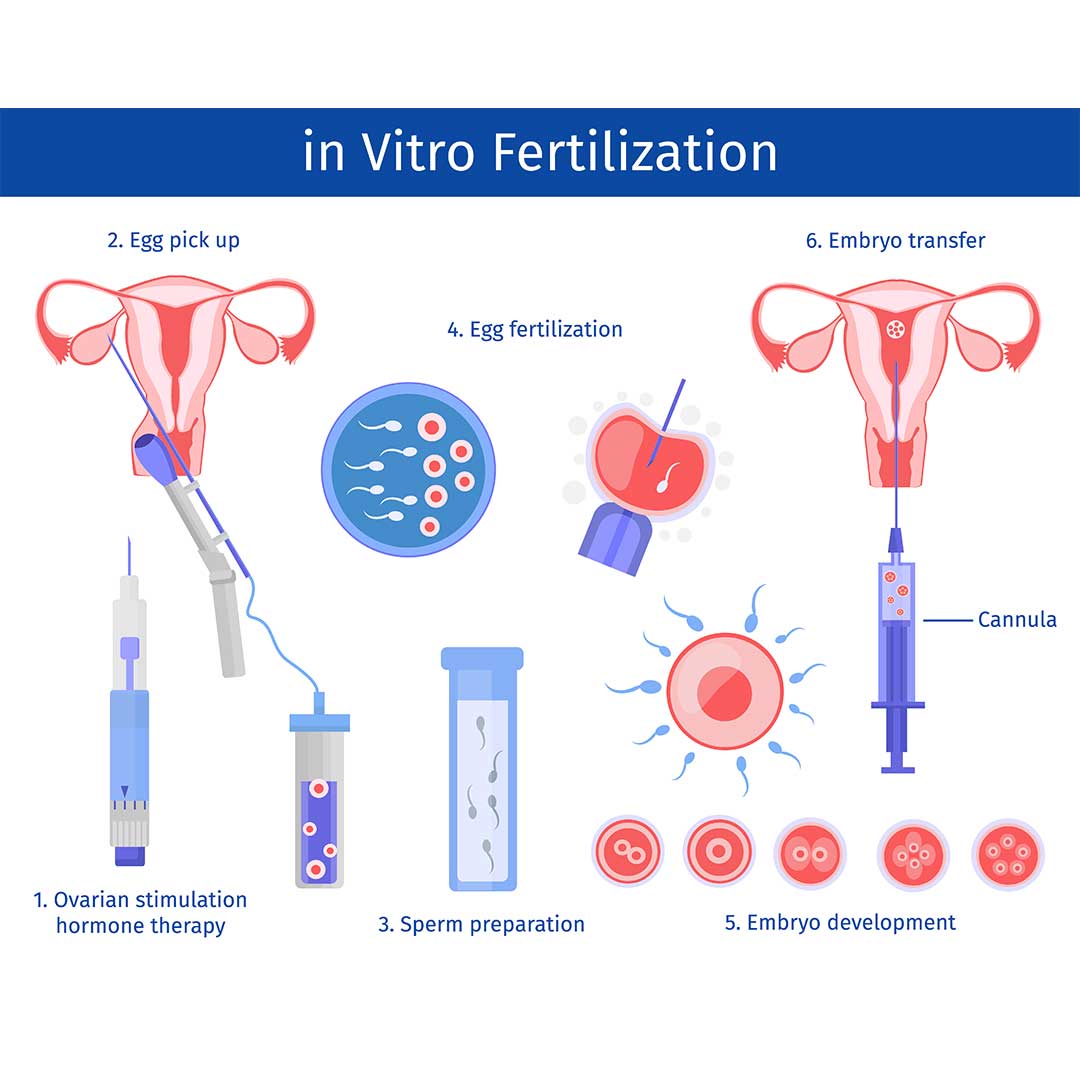
Single women with no current male partner, may choose this option over embryo preservation. The procedure of egg freezing has improved a lot since past decades. Despite the success of egg freezing, pregnancy rates with embryo freezing have been better than egg freezing. Women will be given some medications to grow eggs. Once the eggs are grown, they are collected and immediately frozen. After the cancer treatment, eggs that survive the freeze – thaw process are fertilized with partner’s semen. The resulting embryos are then placed inside the womb.
Embryo cryopreservation
Embryo cryopreservation is most common way of preserving fertility. The ovaries are stimulated by giving some medications, eggs are collected with gentle suction. Then these eggs are fused with partners semen and resulting embryos are grown. These embryos are frozen. Once cancer treatment is over and women is mentally and physically prepared to produce a baby, one or two embryos are transferred into the womb.
Embryo cryopreservation offers best chances of pregnancy.
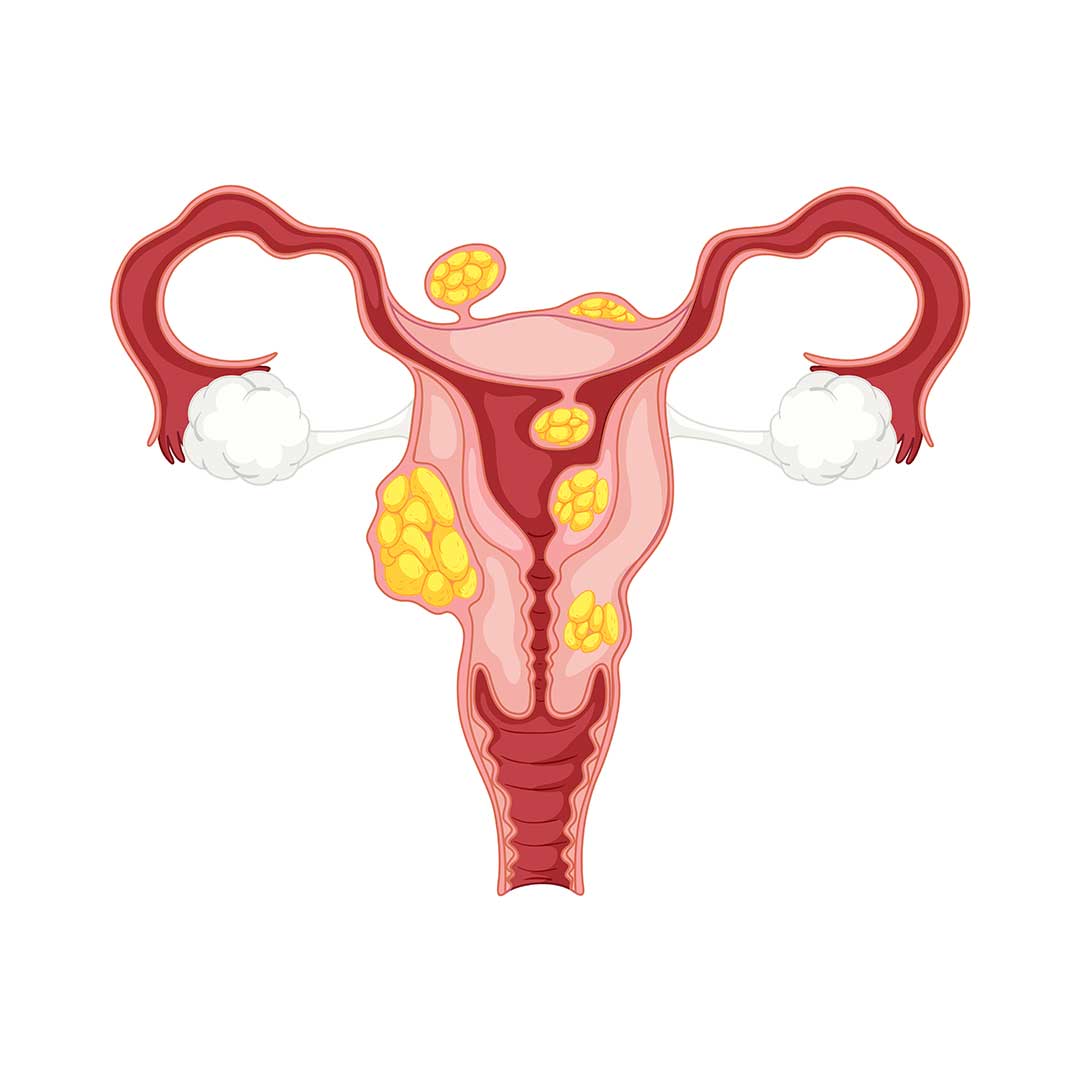
Ovarian tissue cryopreservation
This procedure is under research settings, in which the ovarian tissue that contains resting eggs is cut and sliced and then frozen. After the cancer treatment, this ovarian tissue is thawed and put back into the body. Women may need medications to stimulate this ovarian tissue and produce eggs. This procedure has some disadvantages.
1. It involves multiple surgeries.
2. If the sliced ovarian tissue had cancer cells and is placed back in the body, it may spread cancer.
Hence it is important to know that this is still under research settings, and it has not always been successful at fertility centers.
Dr Megha Gupta,
MBBS,DNB,MICMCH,PGDMLS,FMAS
Fellow of reproductive medicine,
Craft hospital and research centre,
Kodangallur, Kerela.